The good news: most sciatica resolves without surgery. This guide covers what's actually happening in your body, stretches that target the right muscles, sleep positions that help, and what to expect from recovery.
What Is Sciatica?
Sciatica is pain that travels along the sciatic nerve, the longest nerve in your body, which runs from the lower spine through the buttock and down the back of each leg.[1] Unlike localized back pain that stays in one area, sciatica radiates. The pain follows the nerve's path because something is compressing or irritating the nerve root where it exits the spine or along its course through the pelvis.
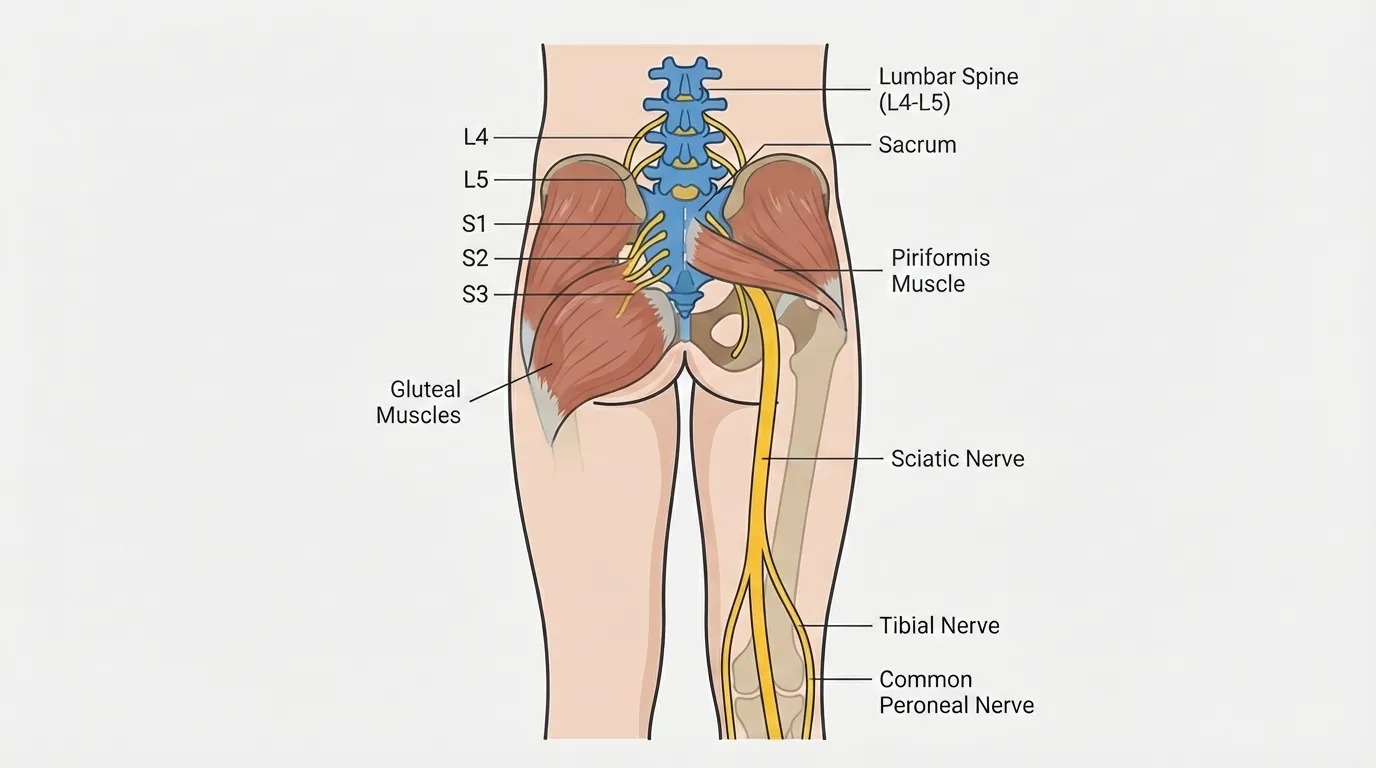
The compression can come from several sources: a bulging disc pressing on the nerve root, a tight piriformis muscle squeezing the nerve in the buttock, or a narrowed spinal canal crowding the nerve as it exits. Understanding which structure is involved matters because each pattern responds to different approaches.
Sciatica affects an estimated 10 to 40 percent of adults at some point in their lives, with the highest rates in people ages 30 to 50.[2] That age range is particularly vulnerable because spinal discs begin losing hydration in the late 20s, making them more prone to herniation, while career demands (long desk hours, commutes) keep the spine under sustained compression. In Miami, where those commutes are longer and desk jobs dominate, the condition is especially common among working-age adults.
Symptoms: How Sciatica Pain Feels
The hallmark of sciatica is pain that shoots from your lower back or buttock down the back of one leg. Many Miami residents first notice it during their morning commute, when sitting in a low car seat for 30-plus minutes makes the burning intensify until they can barely tolerate it.
Common signs include:
- Shooting or burning pain down one leg that may extend to the foot
- Numbness or tingling in the calf, foot, or toes
- Muscle weakness in the affected leg, making it hard to push off when walking
- Pain that worsens with sitting, coughing, or sneezing because these actions increase pressure on the nerve
- Pain that eases with walking or lying down as position changes relieve the compression
Seek immediate medical attention if you experience sudden loss of bowel or bladder control, rapidly progressive leg weakness, or numbness in the groin and inner thighs. These symptoms may indicate cauda equina syndrome, a rare but serious condition that requires urgent surgical evaluation.
What Causes Sciatica?
Sciatica is a symptom, not a diagnosis. Several conditions can compress or irritate the sciatic nerve, and each involves a different mechanism (see our sciatica vs. piriformis vs. disc comparison for a detailed breakdown):
- Herniated disc: The gel-like center of a spinal disc pushes through a crack in the outer wall and presses directly on the nerve root where it exits the spine. This is the most common cause, accounting for roughly 90 percent of sciatica cases.[3]
- Piriformis syndrome: The piriformis muscle in the buttock tightens and compresses the sciatic nerve beneath it. In about 20 percent of people, the nerve actually passes through this muscle rather than beneath it, which means any tightness directly squeezes the nerve instead of just pushing against it.
- Spinal stenosis: The spinal canal gradually narrows with age, crowding the nerve roots. Symptoms tend to worsen with standing and walking and ease when sitting or bending forward.
- Degenerative disc disease: As discs lose height and hydration over time, the space for nerve roots shrinks. This is a slow process, often affecting people over 50.
Why Miami Residents Are at Higher Risk
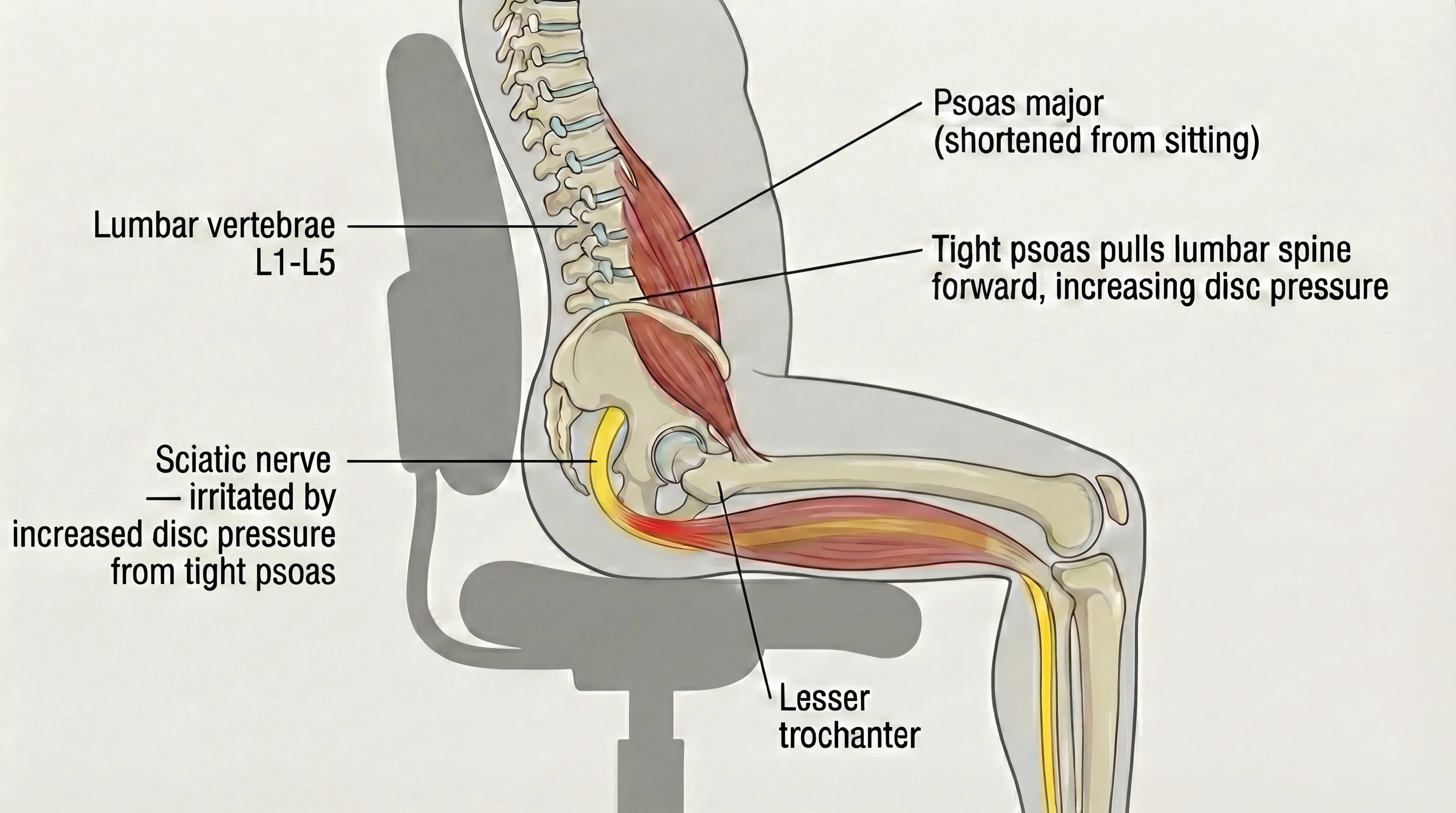
Prolonged sitting is the single biggest modifiable risk factor for sciatica, and Miami's lifestyle puts residents in a chair more than most realize. Sitting loads the lumbar discs at roughly 40 percent more pressure than standing because it removes the spine's natural curve and shifts your weight forward onto the discs instead of distributing it through the joints and muscles behind them.[1] The hip flexors shorten, pulling the pelvis forward and increasing compression on the lower lumbar nerve roots where most sciatica originates.
Long commutes on SW 8th Street and the Dolphin Expressway compound the problem: low car seats put the hips below the knees, increasing lumbar flexion and disc pressure. After 30-plus minutes in that position, stepping out of the car forces the compressed spine to suddenly bear full weight, which can trigger or worsen nerve irritation.
Desk workers in Brickell's financial towers and Wynwood's creative studios face the same pattern in a different seat. Eight hours of hip flexion followed by a commute home means the piriformis rarely gets a chance to lengthen, keeping the sciatic nerve under sustained pressure throughout the day.
There's also a factor most people overlook: the psoas. This deep muscle connects your lumbar spine to your thigh bone and runs through the front of the pelvis. When it shortens from prolonged sitting, it pulls the lower spine forward, compressing the discs from the front while the piriformis and glutes tighten from behind. The nerve gets squeezed from both directions. Most sciatica treatments focus only on the back, but if the front-chain tension isn't addressed, the compression cycle continues.
Managing Sciatica Pain During the Day
Stretches and sleep positioning help at the bookends of your day, but sciatica is often worst during the hours in between: the commute, the desk shift, the moments when you need to get up, sit down, or pick something up off the floor. These adjustments won't resolve sciatica on their own, but they can make the difference between a manageable day and a miserable one.
How to Sit at a Desk with Sciatica
Keep your hips level with or slightly above your knees, feet flat on the floor, and a lumbar support roll behind your lower back. Most office chairs in Brickell and Downtown Miami let the hips sink below the knees, which increases lumbar flexion and disc pressure on the nerve root.
Set a timer to stand and walk for 2 to 3 minutes every 30 minutes. This sounds aggressive, but short movement breaks are the single most effective way to prevent the nerve from staying compressed in one position. Even walking to the water cooler and back counts.
How to Drive with Sciatica
Move your seat forward so your knees stay level with your hips, and place a small lumbar roll or folded towel behind your lower back. Low car seats are one of the worst positions for sciatica because they drop the hips below the knees and round the lumbar spine, increasing disc pressure.
On long commutes down SW 8th Street or the Palmetto, stop every 20 to 30 minutes to stand and do a 30-second standing back extension (hands on hips, lean gently backward). If stopping isn't possible, shift your weight from side to side periodically and avoid crossing the affected leg. For more detail, see our full guide on how to drive with sciatica.

How to Get Out of Bed with Sciatica
Use the log roll technique: roll onto your side, drop your feet off the edge of the bed, and push up with your hands while keeping your spine neutral. Sitting straight up from a lying position forces the spine into flexion, which is exactly the movement that compresses the nerve root.
How to Lift and Bend
Hinge at the hips, not the waist. Bend your knees, keep the object close to your body, and let your legs do the work. Rounding the lower back under load is the most common way to trigger or worsen a sciatica flare. When picking something light off the floor, the golfer's lift (extending one leg behind you as a counterbalance) keeps the spine neutral.
How Sciatica Is Diagnosed
Diagnosing sciatica starts with a physical exam that tests nerve tension and identifies which movements reproduce your symptoms. The straight leg raise test, where your provider lifts your extended leg while you lie on your back, is the most common clinical assessment. If this recreates the shooting pain below the knee, the nerve is likely compressed.
Your provider will also assess muscle strength, reflexes, and sensation in your legs to determine which nerve root is involved. In most cases, imaging is not necessary for the initial evaluation. Many Miami residents start with their primary care doctor, who can perform these tests and refer to a specialist if needed.
When to See a Specialist
Sciatica that persists beyond two weeks of home care, causes progressive leg weakness, or involves numbness in the foot warrants evaluation by a specialist. Warning signs include:
- Leg pain that does not improve or worsens despite rest and stretching
- Progressive weakness in the foot or ankle (difficulty lifting the toes)
- Numbness that spreads to new areas of the leg or foot
- Pain severe enough to disrupt sleep or daily function
Early evaluation helps rule out structural causes that may need specific intervention and prevents acute sciatica from becoming chronic.

Sciatica Treatment Options
Most sciatica responds to conservative treatment. A systematic review found that roughly 90 percent of cases resolve without surgical intervention.[4] The most common options, from least to most intensive:
- Self-care -- rest from aggravating activities, ice or heat, and gentle stretching (covered in detail in the next section)
- Over-the-counter pain relief -- NSAIDs like ibuprofen reduce inflammation around the nerve root for short-term symptom management
- Physical therapy -- strengthening exercises for the core and hip stabilizers to reduce ongoing nerve compression
- TheraMax (robotic muscular therapy) -- sustained, precise pressure designed to target deep restrictions in the piriformis, psoas, and lower back muscles
- Epidural steroid injections -- cortisone delivered directly to the inflamed nerve root for temporary relief (does not address the underlying compression)
- Surgery (microdiscectomy) -- removal of the herniated disc material pressing on the nerve, reserved for cases that fail 6-12 months of conservative care or involve progressive neurological deficits
At-Home and Conservative Care
Most sciatica improves with consistent conservative care. Key strategies:
- Activity modification: Avoid prolonged sitting. Stand, walk, or change positions every 30 to 45 minutes
- Ice therapy: Apply ice for 15-20 minutes to the lower back or buttock during the first 48-72 hours of a flare
- Heat therapy: After the acute phase, moist heat helps relax the tight muscles contributing to nerve compression
- Walking: Short, flat walks (10-15 minutes) promote healthy nerve mobility and reduce stiffness. Bayfront Park offers level paths ideal for this. If heel pain limits your walking, see our plantar fasciitis guide, as the two conditions can overlap
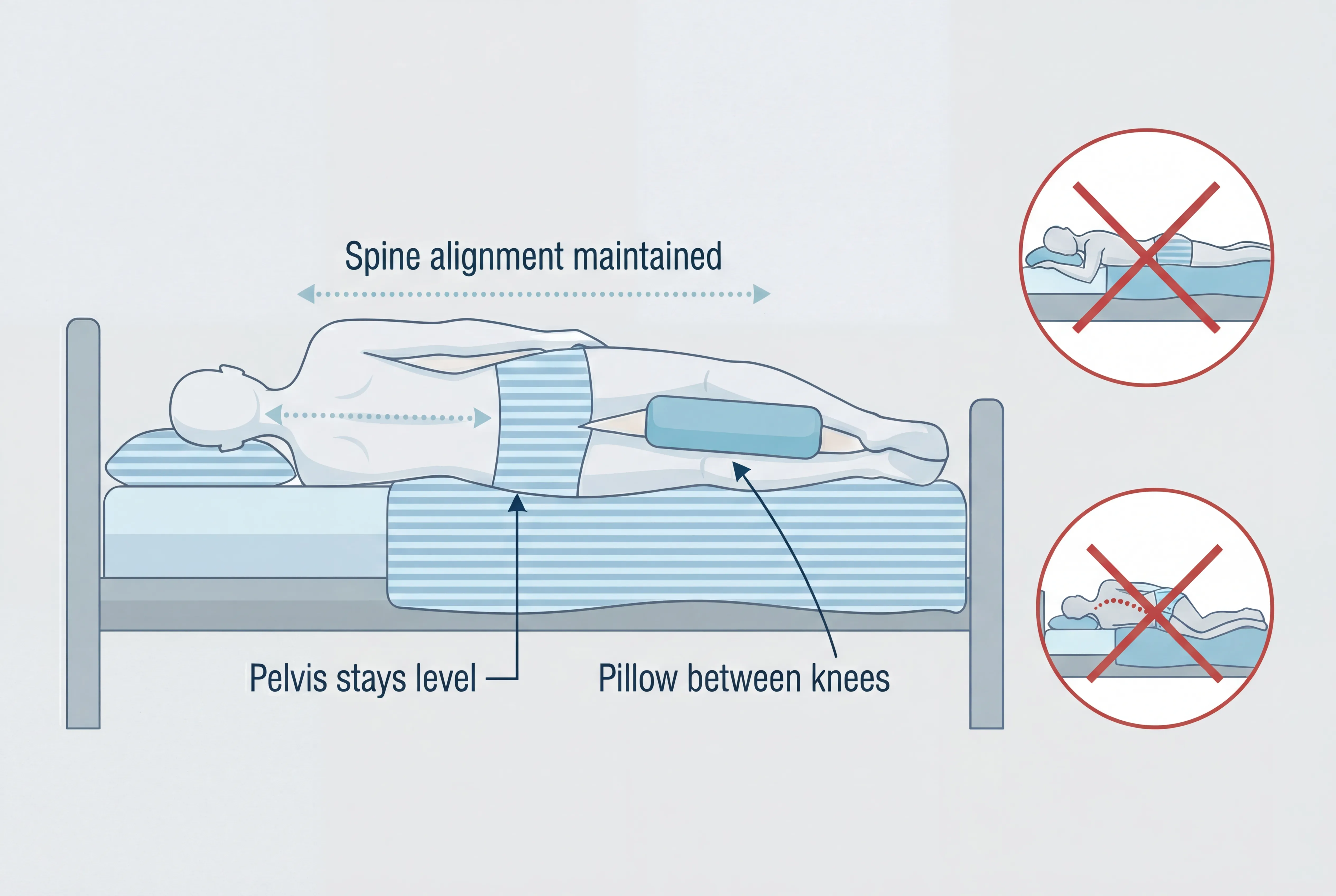
- Sleeping position: Side sleeping with a pillow between the knees maintains neutral spine alignment (covered in detail below)
Quick Relief During a Flare:
Lie on your back with your knees bent and feet flat on the floor. Place a pillow under your knees for support. This position takes pressure off the lumbar discs and often eases the shooting pain within minutes. Stay for 10-15 minutes.
TheraMax Treatment
When home care and stretching stall, TheraMax robotic therapy is designed to target the deep muscular restrictions that are often inaccessible through manual techniques or stretching alone. The approach works along the entire chain of tension, from the psoas and hip flexors in the front to the piriformis and lower back extensors in the back, rather than focusing only on the point of pain.
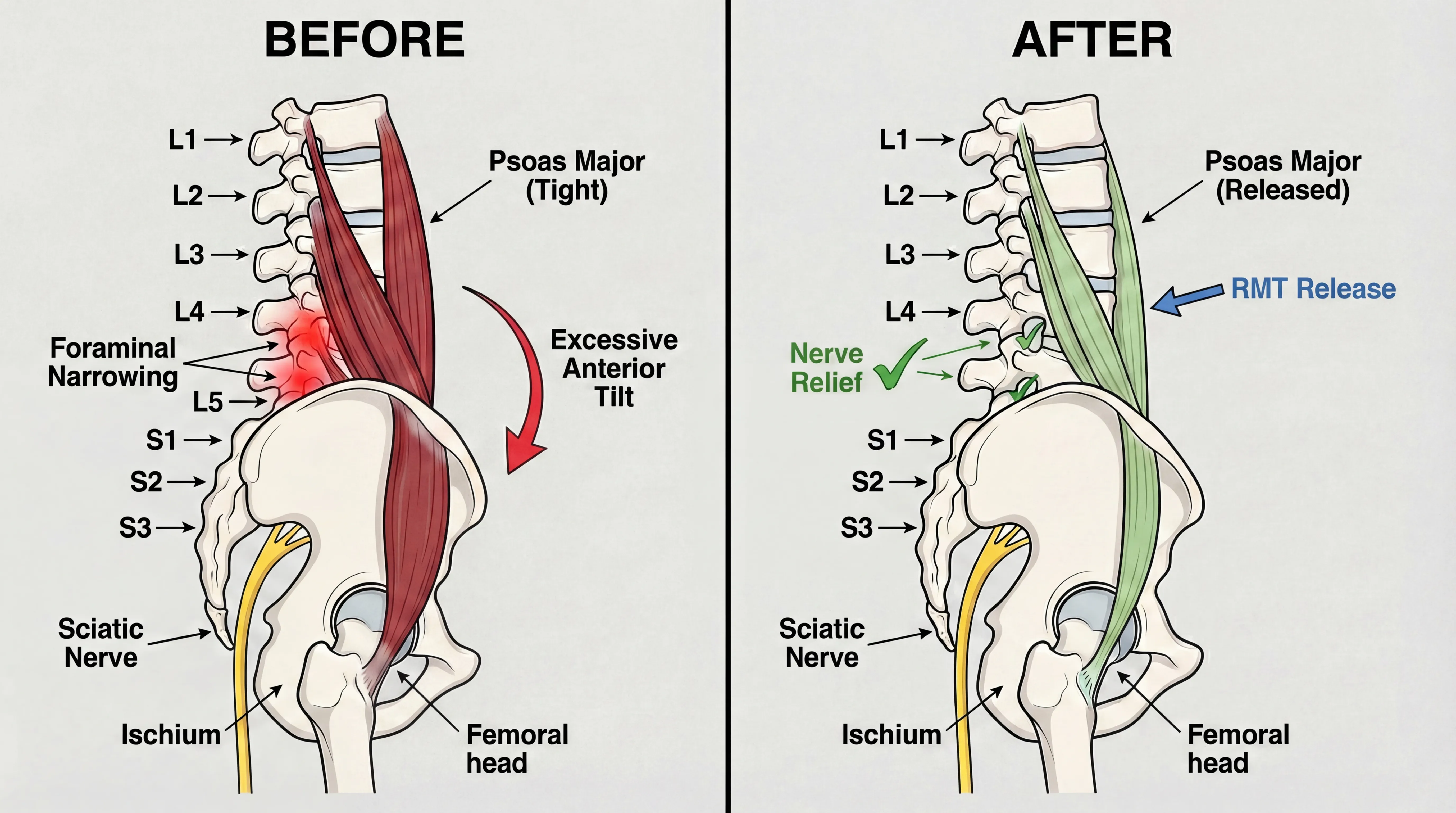
At TheraMax on Coral Way, we evaluate the full posterior chain. Many sciatica clients tell us that previous treatments focused exclusively on their back, missing the psoas and deep hip rotators that were also contributing to nerve compression. TheraMax applies sustained, robotic precision pressure that human hands cannot replicate, designed to release these deep restrictions.
What to expect:
- Pro: Reaches deep muscles (psoas, piriformis, deep rotators) that stretching and manual therapy have difficulty accessing. Consistent pressure across around 6 sessions. Most clients notice a significant change within several sessions. Sciatica typically takes longer than conditions like plantar fasciitis because the muscles involved are larger and have usually been shortened for longer before symptoms appear.
- Con: Not covered by insurance (TheraMax is a cash-pay clinic accepting cash, credit cards, HSA, and FSA). Newer modality with less long-term research than traditional physical therapy.
- Best for: People who have not responded to stretching, PT, or chiropractic alone, or who want targeted deep-tissue work along the full chain.
Learn how we address sciatica at TheraMax or call (786) 480-0026.
When Surgery May Be Considered
Surgery for sciatica is typically reserved for cases that have not improved after 6 to 12 months of consistent conservative care, or for people with progressive neurological deficits like foot drop or worsening leg weakness.[4] The most common procedure, microdiscectomy, removes the portion of herniated disc pressing on the nerve.
Explore every conservative approach first, including physical therapy and targeted muscular therapy, before discussing surgery with your doctor.
Best Stretches for Sciatica
Stretching for sciatica targets two goals: loosening the muscles that compress the nerve and mobilizing the nerve itself so it glides freely through surrounding tissue. Consistency matters more than intensity. Do these daily, holding each stretch for 30 seconds unless noted otherwise.[5]
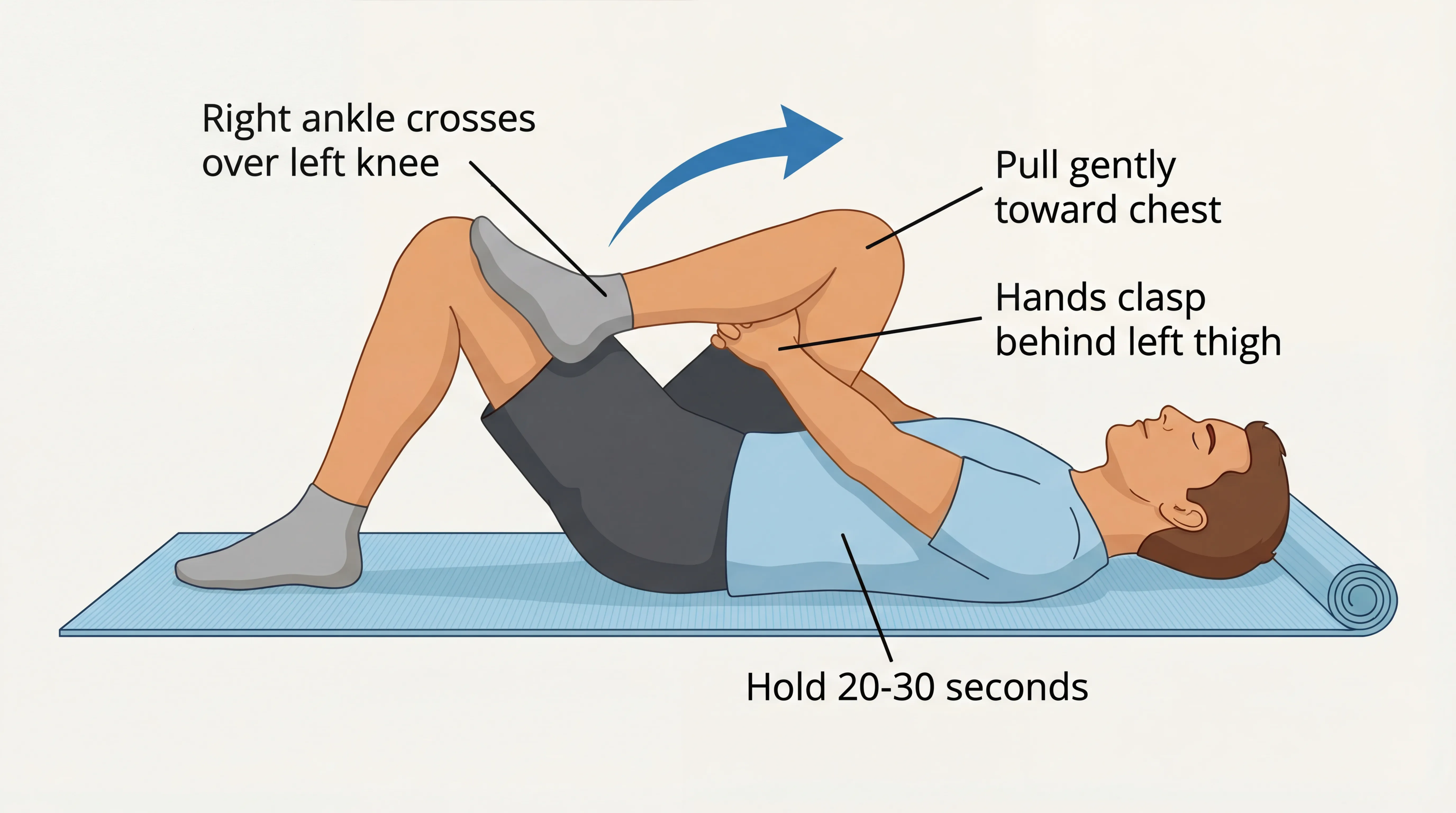
Piriformis Stretch (Figure-4)
Lie on your back, cross the affected leg over the opposite knee to form a figure-4, then pull the bottom knee toward your chest. Hold 30 seconds. Repeat 3 times.
This targets the piriformis muscle directly. If the piriformis is contributing to your sciatica, you should feel a deep stretch in the buttock of the crossed leg. Miami residents who sit in low car seats for long commutes often find this stretch provides the most immediate relief.
Sciatic Nerve Glide
Sit on a chair, straighten the affected leg with foot flexed toward you, then slowly point the toes away. Repeat 10 times in a gentle pumping motion. Do not hold at end range.
Unlike a stretch, a nerve glide moves the nerve through the surrounding tissue rather than putting it under sustained tension. This reduces adhesions that develop when the nerve is compressed. The motion should feel like a gentle pull, not a sharp reproduction of your sciatica symptoms. If it recreates the shooting pain, reduce the range of motion.
Knee-to-Chest Stretch
Lie on your back, pull one knee to your chest while keeping the other foot flat on the floor. Hold 30 seconds per side. Repeat 3 times.
This opens the lumbar spine and gently separates the vertebrae, reducing pressure on the nerve root where it exits the spine. It also stretches the lower back extensors that often tighten to guard an irritated nerve.
Cat-Cow (Spinal Mobilization)
Start on hands and knees. Arch your back upward (cat) then let it sag toward the floor (cow). Move slowly through 10 repetitions.
This mobilizes the entire lumbar spine through flexion and extension, pumping fluid into the discs and loosening the muscles on both sides of the spine. Many people with sciatica find that the first few repetitions feel stiff, but the movement loosens progressively.
When to Stretch:
Stretch first thing in the morning before standing, after long periods of sitting, and after any exercise. If you walk at Bayfront Park or cycle along the Rickenbacker Causeway, stretch the piriformis and hamstrings before and after every outing. Consistency matters more than intensity.
Sciatica Recovery Timeline
Recovery time depends on the underlying cause, severity, and how you approach treatment. Here's what to expect.
| Approach | Typical Timeline | Best For |
|---|---|---|
| Self-care alone | 4-12 weeks | Mild, first-episode sciatica with no neurological symptoms |
| TheraMax | ~6 sessions | Persistent sciatica involving deep muscle restrictions (psoas, piriformis) |
| Surgery (microdiscectomy) | 6-12 month recovery | Failed conservative care or progressive neurological deficits |
With Self-Care Alone: 4-12 Weeks
Most sciatica cases improve within 4 to 12 weeks with consistent stretching, activity modification, and patience.[1] The wide range depends on whether the cause is muscular (piriformis, faster) or disc-related (slower). For a week-by-week breakdown, see how long does sciatica last.
Weeks 1-2: Focus on pain management. Ice, gentle nerve glides, and avoiding aggravating positions. The shooting pain may fluctuate day to day.
Weeks 3-4: Pain typically decreases in frequency and intensity. Stretching becomes easier. Light walking and daily activities feel more manageable.
Weeks 5-8: Most people are walking comfortably and sitting for longer periods without flares. Strengthening exercises can begin.
Weeks 8-12: Full recovery for many cases. The nerve pain is gone or occasional. Maintenance stretching and proper ergonomics prevent recurrence.
With TheraMax: Significantly Faster
Self-care works on the surface. TheraMax reaches the deep restrictions in the psoas, piriformis, and hip rotators that stretching alone cannot access, which may help support a faster recovery. Sciatica involves larger, deeper muscles than many other conditions, which is why it typically requires more sessions, but most clients notice a meaningful shift within the first few visits.

Return to Activity Protocol
Returning to full activity too soon is the most common reason sciatica comes back after treatment. Follow a gradual progression:
- Start with short, flat walks at places like Crandon Park, where the paved paths offer level terrain ideal for early recovery
- Add piriformis and hamstring stretches daily, especially before and after walking
- Introduce core strengthening (modified planks, bird dogs) once walking is pain-free
- Resume recreational activities at 50% intensity, whether that's golf at the Biltmore or tennis at Flamingo Park
- Monitor symptoms: Any return of shooting leg pain means you've progressed too fast. Scale back and allow more time
Sleeping with Sciatica
Sleep is when your body repairs, but the wrong position can keep the sciatic nerve compressed for eight hours straight. In Miami, where air conditioning drops overnight temperatures significantly, the cold can increase tissue stiffness around the nerve and make morning symptoms worse.
Best positions:
- Side sleeping with a pillow between the knees: This keeps the pelvis level and prevents the top leg from pulling the spine into rotation, which compresses the nerve root. Sleep on the unaffected side when possible.
- Back sleeping with a pillow under the knees: This flattens the lumbar curve and reduces disc pressure on the nerve root. A small rolled towel under the lower back provides additional support.
Worst position:
- Stomach sleeping: Forces the lower back into extension, narrowing the space where nerve roots exit the spine. If you can't break the habit, place a thin pillow under your hips to reduce the arch.
Morning routine: Before getting out of bed, do 3 gentle knee-to-chest pulls and 10 cat-cow repetitions. This mobilizes the spine and circulates fluid into the discs before they have to bear your weight. Then stand slowly and take your first steps deliberately.
Preventing Sciatica
Once sciatica resolves, prevention focuses on addressing the factors that caused the compression in the first place. For Miami residents, that usually means countering the effects of prolonged sitting and building core stability.
Practical prevention tips:
- Stand or walk for 5 minutes every 30 minutes if you work at a desk in Brickell, Downtown, or Wynwood. Set a timer.
- Strengthen your core: Modified planks, dead bugs, and bird dogs stabilize the spine and reduce the load on lumbar discs. Three sessions per week is enough.
- Stretch your hip flexors daily: The psoas shortens during sitting and pulls the pelvis forward, increasing disc pressure. A kneeling hip flexor stretch held for 30 seconds per side counteracts this.
- Swim: Miami's warm climate and year-round pool access make swimming one of the best exercises for sciatica prevention. Buoyancy eliminates spinal compression while allowing full-range movement. Biscayne Bay and local pools offer options year-round.
- Maintain a healthy weight: Excess weight increases the load on lumbar discs, accelerating degeneration and increasing herniation risk.
- Use proper lifting mechanics: Bend at the hips and knees, not the waist. Keep the load close to your body. This protects the discs from the asymmetric pressure that causes herniations.
Sciatica FAQ
Sciatica is one of the most common causes of leg pain in adults. The following answers address questions Miami residents ask most often about exercise, recurrence, and related conditions.
1 Can I exercise with sciatica, or should I rest?
2 How is sciatica different from general lower back pain?
3 Will my sciatica come back after it heals?
4 Does sciatica affect both legs at the same time?
5 Can I do TheraMax Robotic Therapy while in physical therapy?
References
- Sciatica. N Engl J Med. 2015 . PubMed
- Sciatica: review of epidemiological studies and prevalence estimates. Spine. 2008 . PubMed
- Sciatica. Best Pract Res Clin Rheumatol. 2010 . PubMed
- Comparative clinical effectiveness of management strategies for sciatica. Spine J. 2015 . PubMed
- Advice to stay active or structured exercise in the management of sciatica. Spine. 2015 . PubMed


