The good news: most people recover without surgery. This guide covers what causes plantar fasciitis, how to manage it at home, and when to seek professional help.
What Is Plantar Fasciitis?
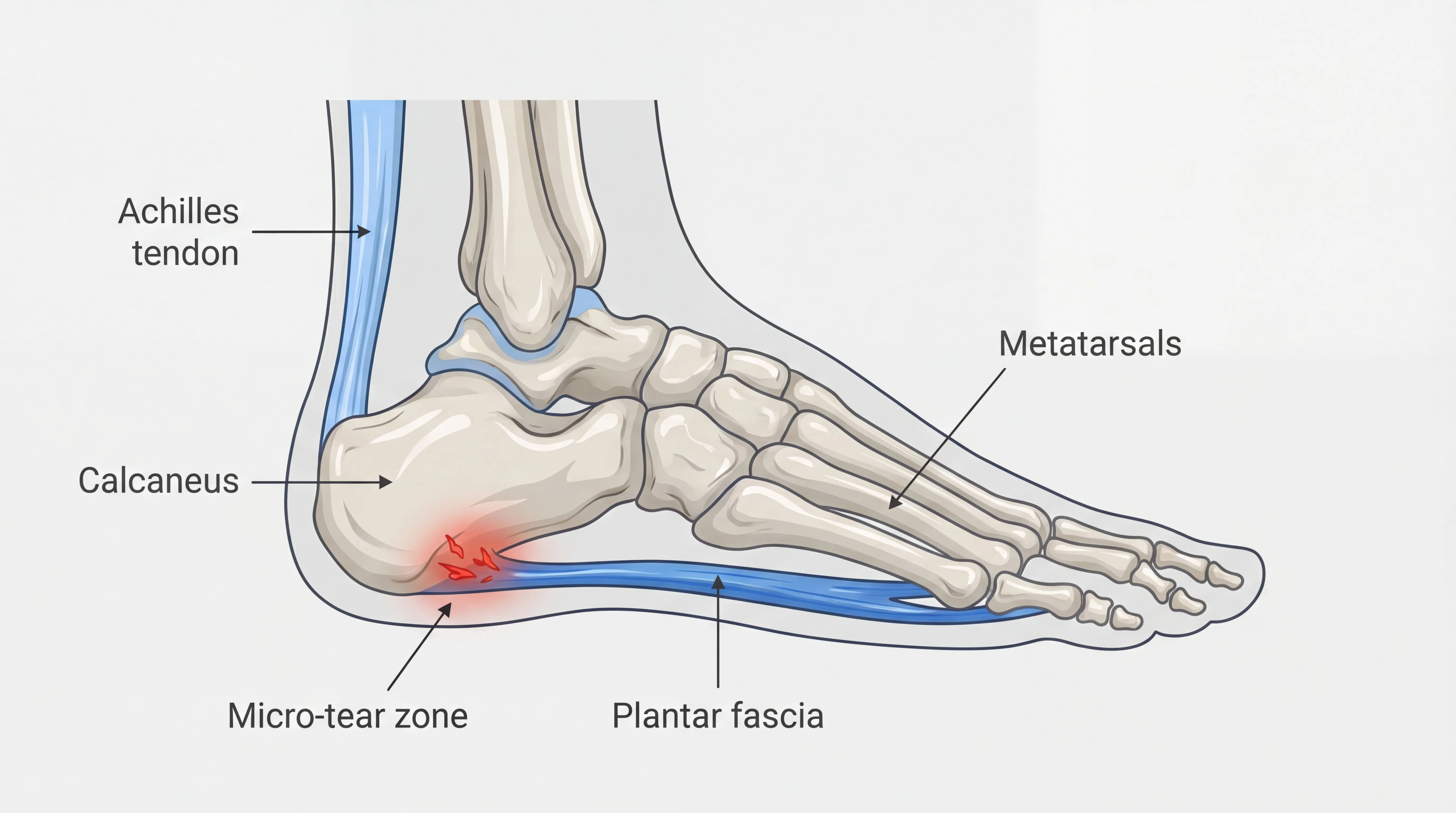
Plantar fasciitis is a degenerative condition of the plantar fascia, the thick band of tissue that runs along the bottom of your foot from the heel bone to the toes.[3] This tissue supports your arch and absorbs shock with every step you take.
When overstressed, the fascia develops small tears and stiffens. Overnight, your feet relax into a pointed position that lets the damaged tissue contract. Your first morning step forces it to stretch suddenly against that tightness, which is why the pain hits hardest when you get out of bed.
Plantar fasciitis accounts for over one million doctor visits per year in the U.S.[2] and is especially common in adults ages 40 to 60. In Miami's warm climate, where sandals and flip-flops are year-round footwear, the condition is particularly prevalent.
Symptoms: How Plantar Fasciitis Heel Pain Feels
The hallmark symptom is heel pain that peaks with your first steps of the day and returns after long periods off your feet. Many Miami residents first notice it stepping onto tile or terrazzo floors in the morning.
Common signs include:
- Heel pain that peaks with your first morning steps and gradually eases with movement
- Pain that returns after sitting or standing for long periods
- A burning or aching sensation along the bottom of your foot
- Pain that worsens during activity and eases with rest
Go to the ER or call your doctor if you experience sudden, severe foot pain after an injury, heel pain with fever or swelling, or numbness and tingling in your foot. These may indicate a fracture, infection, or nerve condition.
What Causes Plantar Fasciitis?
Plantar fasciitis develops when repeated mechanical stress creates small tears in the plantar fascia tissue. Tight calf muscles and inadequate footwear increase tension on the fascia and contribute to chronic heel pain over time.
Several factors raise your risk:
- Tight calf muscles and Achilles tendons that pull on the fascia from above
- Improper footwear, especially flip-flops and sandals that lack arch support
- High-impact activities like running or jumping on hard surfaces
- Occupations requiring prolonged standing
- Age 40-60, when the fascia loses elasticity
- Excess body weight, which adds load to the fascia
Why Miami Residents Are Especially At Risk
Miami residents face elevated plantar fasciitis risk because year-round flip-flop wear removes arch support and hospitality jobs require prolonged standing on hard floors. Long Dolphin Expressway commutes compound the problem: sitting for 30-plus minutes tightens the calves, and then stepping out of the car forces the stiffened fascia to bear your full weight at once.
Workers in Aventura's hospitality industry and Brickell's service sector are especially vulnerable. The sit-then-stand commute cycle compresses the calf, then stretches the tight fascia, restarting the pain cycle. This pattern can also contribute to shin splints.

Plantar Fasciitis vs. Heel Spurs
Plantar fasciitis is pain from the soft tissue (the fascia); a heel spur is a bony calcium deposit on the heel bone. They often coexist but require different attention.
Heel spurs develop as a result of chronic plantar fasciitis but do not always cause pain on their own.
Heel spurs frequently show up on X-rays but produce no symptoms on their own. Plantar fasciitis is almost always the actual source of that sharp morning heel pain. Treatment for both conditions starts the same way: reducing tension on the fascia through stretching, supportive footwear, and targeted therapy.
How Plantar Fasciitis Is Diagnosed
Diagnosing plantar fasciitis starts with a physical exam and a review of your symptoms and activity level. Your provider checks for tenderness along the heel and arch, evaluates your foot mechanics, and may assess your gait.
Imaging is not usually necessary, but persistent heel pain may require an X-ray to rule out stress fractures or heel spurs.
When to See a Specialist
Persistent heel pain lasting more than two weeks despite rest, pain severe enough to limit walking, or numbness and swelling in your foot are signs that you should see a specialist for plantar fasciitis evaluation.
Warning signs include:
- Heel pain lasting more than two weeks despite rest
- Pain severe enough to limit walking or daily activities
- Numbness, tingling, or swelling in your foot
- Pain that gets worse rather than better over time
Early intervention leads to faster recovery and helps prevent chronic heel pain.
Plantar Fasciitis Treatment Options
Plantar fasciitis responds well to conservative treatment, with more than 90 percent of cases recovering without surgery.[1] The most common treatment options, from least to most intensive:
- Self-care -- stretching, ice, night splints, and supportive footwear
- Orthotics -- custom or over-the-counter insoles to redistribute pressure
- Cortisone injections -- short-term inflammation relief (does not address the underlying cause)
- TheraMax (robotic muscular therapy) -- designed to release the deep calf, Achilles, and fascial restrictions contributing to the pain cycle
- Extracorporeal shock wave therapy (ESWT) -- sound waves to stimulate healing in chronic cases
- Surgery -- partial plantar fascia release, reserved for cases that fail 6-12 months of conservative care
At-Home and Conservative Care
Most plantar fasciitis responds to conservative home care without professional treatment. Key self-care strategies:
- Rest and activity modification to reduce stress on the fascia
- Ice therapy for 15-20 minutes after activity to calm inflammation
- Supportive footwear with proper arch support (avoid flat sandals and flip-flops)
- Night splints to prevent the fascia from tightening while you sleep
- Over-the-counter anti-inflammatories for short-term pain management
Quick Relief Between Sessions:
Roll a frozen water bottle under your foot for 10 minutes after a long day of standing. The combination of cold therapy and gentle massage helps reduce pain and stiffness.

Professional Therapy
When home care stalls, professional treatment targets the deep tissue restrictions that stretching cannot reach. TheraMax robotic therapy is designed to work along the entire posterior chain rather than the heel alone, addressing the tension pattern that contributes to recurring pain.
TheraMax reviews the entire chain from pelvic tilt to calf tightness to plantar fascia, not just the point of pain. Learn how we treat plantar fasciitis or call (786) 480-0026.
When Surgery May Be Considered
Surgery for plantar fasciitis is rarely needed and is typically considered only after 6 to 12 months of consistent conservative care have failed to resolve symptoms. Fewer than 10 percent of plantar fasciitis cases ever require a surgical procedure.[1]
Explore every conservative approach first, including targeted therapy and home exercise programs, before discussing surgery with your doctor.
Best Stretches for Plantar Fasciitis
Consistent daily stretching is one of the most effective ways to manage plantar fasciitis at home.[4] The best results come from stretches targeting three areas: the calf muscles, the Achilles tendon, and the plantar fascia itself.
Calf Wall Stretch
Stand facing a wall, one foot back, heel flat on the ground. Lean forward and hold 30 seconds per side. Repeat 3 times.
This loosens the gastrocnemius muscle, which pulls on the Achilles tendon and plantar fascia from above. You should feel a deep stretch in the back of your lower leg, not pain.

Towel Stretch (Morning Routine)
Before getting out of bed, loop a towel around the ball of your foot and gently pull your toes toward you. Hold 30 seconds.
This warms up the fascia before your first steps and reduces that morning pain. Especially helpful in Miami, where cool tile and terrazzo floors make those first barefoot steps worse.
Plantar Fascia Roll
Sit in a chair and roll a tennis ball or frozen water bottle under the arch of your foot for 2 to 3 minutes with moderate pressure.
This breaks up tightness along the fascia and provides immediate relief.
Eccentric Calf Raise
Stand on a step with heels hanging off the edge. Slowly lower your heels below the step over 3 to 5 seconds. Rise back up. Repeat 10 to 15 times.
Research shows that eccentric loading strengthens the calf and Achilles tendon, reducing the tension they transfer to the plantar fascia.[5]
When to Stretch:
Stretch your calves and feet first thing in the morning, before and after exercise, and after long periods of sitting. If you run along the Rickenbacker Causeway or walk at Tropical Park, stretch before and after every outing. Consistency matters more than intensity.
Plantar Fasciitis Recovery Timeline
Recovery time depends on how you treat it. Here's what to expect with self-care alone versus professional treatment.
With Self-Care Alone: 6-12 Weeks
Most plantar fasciitis cases improve within 6 to 12 weeks with consistent stretching, icing, and supportive footwear. Full recovery depends on severity, how long symptoms have persisted, and adherence to your care plan.
Weeks 1-2: Focus on rest, ice, and gentle stretching. Morning pain and daily discomfort begin to ease.
Weeks 3-4: Strengthening exercises begin as tension releases. Light walking and low-impact activities return.
Weeks 5-8: Gradual return to normal routines. Most people are walking comfortably and resuming exercise.
Weeks 8-12: Full recovery for most cases. Maintenance stretching and proper footwear prevent recurrence.
With TheraMax: Significantly Faster
Self-care works on the surface. TheraMax is designed to reach the deep calf, Achilles, and fascial restrictions that stretching alone cannot address, compressing the recovery timeline.
Return to Activity Protocol
Rushing back to full activity too soon is the most common reason plantar fasciitis returns after treatment. A gradual return protocol that increases distance by no more than 10 percent per week, combined with daily stretching and supportive footwear, prevents recurrence.
Follow these guidelines:
- Start with short, flat walks before adding distance
- Stretch your calves and feet daily, especially before morning steps
- Increase activity by no more than 10% per week
- Wear supportive shoes during all weight-bearing activity
- Listen to your body: if heel pain returns, scale back
The paved paths at Crandon Park on Key Biscayne offer level terrain ideal for a gradual return to outdoor activity.

Sleeping with Plantar Fasciitis
Sleep is when your plantar fascia contracts and stiffens, which is why morning heel pain is the hallmark symptom. In Miami, where many homes rely on air conditioning that drops overnight temperatures sharply, the cold can increase tissue stiffness and make those first steps even worse.
Night splints hold your foot in a slightly flexed position while you sleep, keeping the fascia gently stretched. They feel awkward at first, but most people adjust within a few nights. A sock-style night splint is less bulky than a boot-style and easier to tolerate long-term.
Sleep positioning matters too. Avoid sleeping with your feet pointed downward (plantar flexion), which shortens the calf and fascia overnight. If you sleep on your back, prop a pillow under your calves to keep your feet in a neutral position. Side sleepers can tuck a pillow between their ankles.
Morning routine: Before your feet hit the floor, do the towel stretch described above. Flex and extend your toes 10 to 15 times. Then stand up slowly and take your first steps gently. This 60-second routine can significantly reduce morning pain.
Preventing Plantar Fasciitis
Preventing plantar fasciitis requires consistent attention to footwear, daily stretching habits, and gradual activity progression. Supportive shoes with proper arch support protect the plantar fascia during long periods of standing, walking, or running on hard surfaces.
Practical prevention tips for Miami residents:
- Choose shoes with arch support over flat sandals, even in warm weather. Recovery sandals with contoured footbeds are a good compromise for Miami's climate
- Stretch your calves and Achilles daily, especially after prolonged sitting
- Increase running or walking distance gradually, no more than 10% per week
- Maintain a healthy weight to reduce load on the plantar fascia
- Be cautious with soft sand walking at the beach, which can strain the arch if overdone
Paved paths along the Venetian Causeway and around Coral Gables' Granada Golf Course offer controlled, flat terrain for staying active without overloading the arch.
Plantar Fasciitis FAQ
Plantar fasciitis is one of the most common causes of heel pain in adults. The following answers address the questions Miami residents ask most about exercise, footwear, recurrence, and related conditions.
1 Can I still run or exercise with plantar fasciitis?
2 Are flip-flops really that bad for plantar fasciitis?
3 Can plantar fasciitis come back after it heals?
4 What is the difference between plantar fasciitis and Achilles tendonitis?
References
- Plantar Fasciitis. StatPearls Publishing. 2024 . PubMed
- Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004 . PubMed
- Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003 . PubMed
- Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. J Bone Joint Surg Am. 2003 . PubMed
- High-load strength training improves outcome in patients with plantar fasciitis: a randomized controlled trial with 12-month follow-up. Scand J Med Sci Sports. 2015 . PubMed


