You have pain shooting down your leg, maybe after a long commute on I-95 or a weekend run through Bayfront Park, and you have probably heard multiple possible explanations: sciatica, piriformis syndrome, a herniated disc, a bulging disc.
The confusion is not your fault. These four conditions produce similar symptoms because they all affect the sciatic nerve. The difference is where the problem starts: in a muscle, in a disc, or somewhere else along the nerve's path.
Quick Comparison Overview
Sciatica is a symptom you feel; piriformis syndrome starts in a hip muscle; herniated discs involve a cracked disc wall; bulging discs involve a weakened but intact wall. The table below shows how these differences play out.
| Condition | What it is | Pain location | Key differentiator | Treatment approach |
|---|---|---|---|---|
| Sciatica | A symptom: pain along the sciatic nerve | Lower back through buttock and down the leg | Always has an underlying cause (disc, muscle, or other) | Depends entirely on the cause |
| Piriformis Syndrome | A muscle in the buttock compressing the sciatic nerve | Deep, aching pain concentrated in the buttock | Sitting on hard surfaces makes it significantly worse | Targeted muscle release and hip stretching |
| Herniated Disc | A crack in the disc wall lets inner material push out | Lower back radiating into the leg in a specific pattern | Coughing or sneezing sharpens the leg pain | Core stabilization and possible medical intervention |
| Bulging Disc | The disc wall extends outward but stays intact | Lower back stiffness, mild radiation at most | Often produces no symptoms at all | Conservative care and monitoring |
What Each Condition Actually Is
These four conditions get confused because they all involve the same nerve, but each one starts in a different place. Knowing where your problem actually sits is the fastest way to stop chasing the wrong treatment.
Sciatica
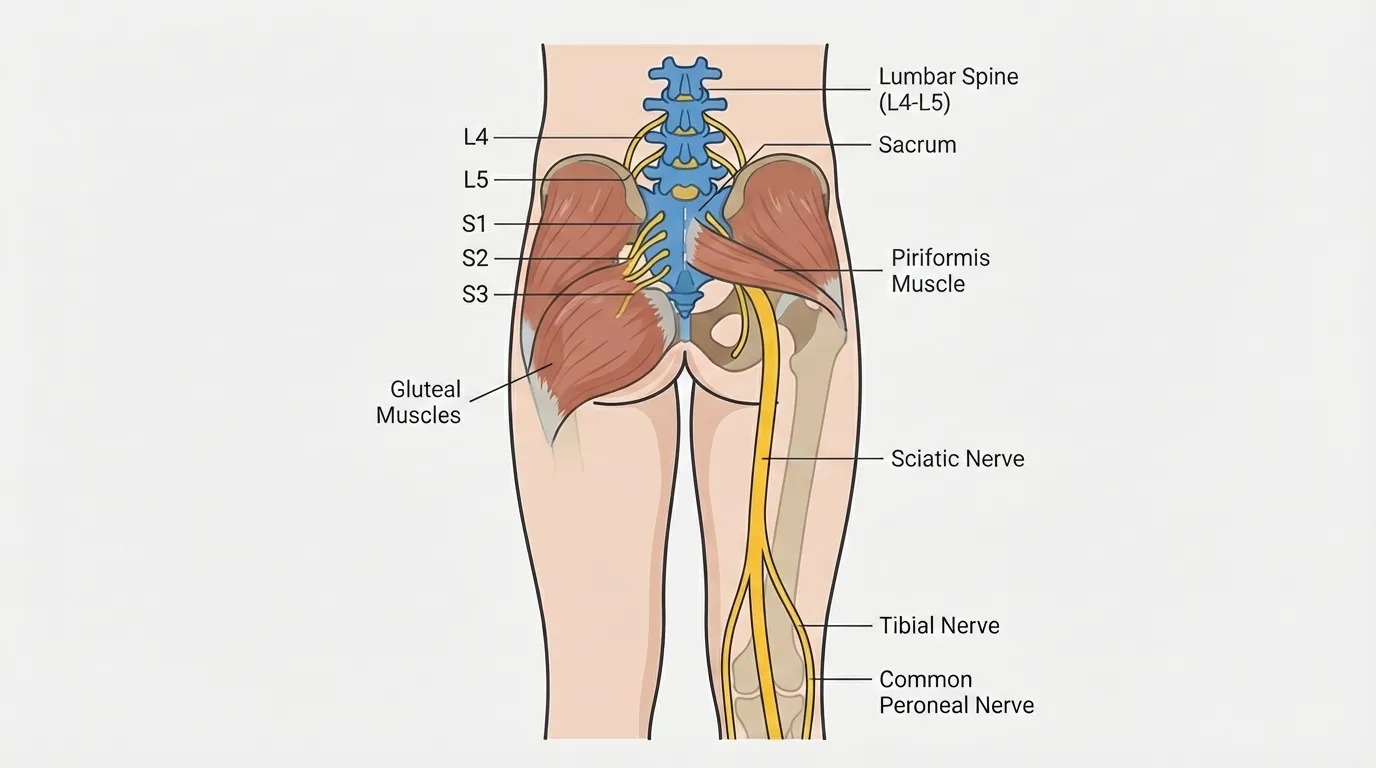
Sciatica is a symptom, not a condition. It's the pain you feel traveling from your lower back down your leg, following the sciatic nerve from the lower spine (L4 through S3) all the way to your foot. About 90% of cases trace back to a disc problem, and piriformis syndrome accounts for roughly 6%.[1]
Think of sciatica as what you feel. The other three conditions are what may be causing it. Learn more in our full sciatica guide.
Piriformis syndrome
Your piriformis is a flat, band-like muscle buried deep under your glute. When it tightens, it squeezes the sciatic nerve against the bone underneath. In about 15% of people, the nerve actually passes through the muscle instead of beneath it, which makes compression even more likely.
Prolonged sitting is a common trigger because sustained hip flexion holds the piriformis in a shortened, contracted state, and the nerve gets compressed between the tensed muscle and the underlying bony pelvis. Miami's desk-heavy workforce in Brickell and Downtown makes this one of the most frequent patterns we see in our clinic. True primary piriformis syndrome is relatively rare; the muscle often tightens as a secondary response to a disc problem. Read more in our piriformis syndrome guide.
Herniated disc
A herniated disc happens when the tough outer wall of a spinal disc cracks and the softer material inside pushes through, most commonly at L4-L5 or L5-S1. The protruding material presses on the nerve root and triggers a chemical inflammatory response.[3] Herniated discs typically affect people between ages 30 and 50, when spinal discs have lost enough hydration to become brittle but the spine is still under heavy daily loading from work and activity. See our herniated disc guide.
Bulging disc
A bulging disc extends beyond its normal boundary, but the outer wall stays intact. Mayo Clinic compares it to "a hamburger that is too big for its bun."[5]
Bulging discs develop gradually as the disc loses water content with age, causing the outer wall to weaken. They are frequently asymptomatic, discovered incidentally on imaging. For more detail, see our herniated and bulging disc guide.
Symptoms Side by Side
All four can give you leg pain, numbness or tingling, and that familiar worsening when you've been sitting too long. What separates them is where your pain starts, what makes it flare, and whether it travels below your knee.
The numbness that creeps in after sitting through a Heat game at Kaseya Center or a long flight into MIA? Any of these four could be behind it. The table below shows which specific patterns point to which diagnosis.
Symptoms that help you tell them apart
| Symptom pattern | Most likely condition |
|---|---|
| Deep, aching pain concentrated in the buttock | Piriformis syndrome |
| Pain shoots below the knee all the way to the foot | Disc-related sciatica (herniation or large bulge) |
| Coughing or sneezing sharpens the leg pain | Herniated disc |
| Pain worsened dramatically by sitting on hard surfaces | Piriformis syndrome |
| Numbness in one specific area of the leg or foot | Herniated disc (follows a dermatomal pattern) |
| Mild, diffuse back stiffness without any leg pain | Bulging disc |
| No symptoms at all, discovered on imaging | Bulging disc |
How to Tell Which One You Have
Start by locating where your pain originates: deep in the buttock points toward piriformis syndrome, lower back radiating into the leg points toward a disc problem, and lower back only suggests a bulging disc. Three branching questions and four self-tests below will sharpen that initial read.
Important: These self-assessments help narrow your possibilities but do not replace professional diagnosis. If your symptoms include progressive weakness, numbness spreading to new areas, or any loss of bladder or bowel control, seek medical evaluation immediately.
Start with three questions
Question 1: Where does your pain start?
- Deep in the buttock (not the lower back): Points toward piriformis syndrome. Move to Question 2.
- Lower back, radiating into the leg: Points toward a disc problem. Move to Question 3.
- Lower back only, no leg pain: May indicate a bulging disc or mechanical back pain.
Question 2: Does sitting on a hard surface make it significantly worse, and does standing or walking ease it?
If sitting on a hard surface makes it worse and standing eases it, piriformis syndrome is the most likely explanation. Try the self-tests below to confirm. If not, a disc problem could be the primary contributor driving the muscle to tighten in response.
Question 3: Does coughing, sneezing, or bearing down sharpen the pain in your leg?
If it does, that points toward a herniated disc. Coughing and sneezing spike intra-abdominal pressure, which transfers directly to the discs and pushes herniated material harder against the nerve root. If coughing has no effect on your leg pain, a milder disc bulge or chemical irritation without significant mechanical compression is more likely.
Four self-tests to try
1. Piriformis palpation test
Press firmly into the deep buttock, midway between the tailbone and hip bone. If this reproduces your shooting leg pain, piriformis involvement is likely.
2. FAIR test (Flexion, Adduction, Internal Rotation)
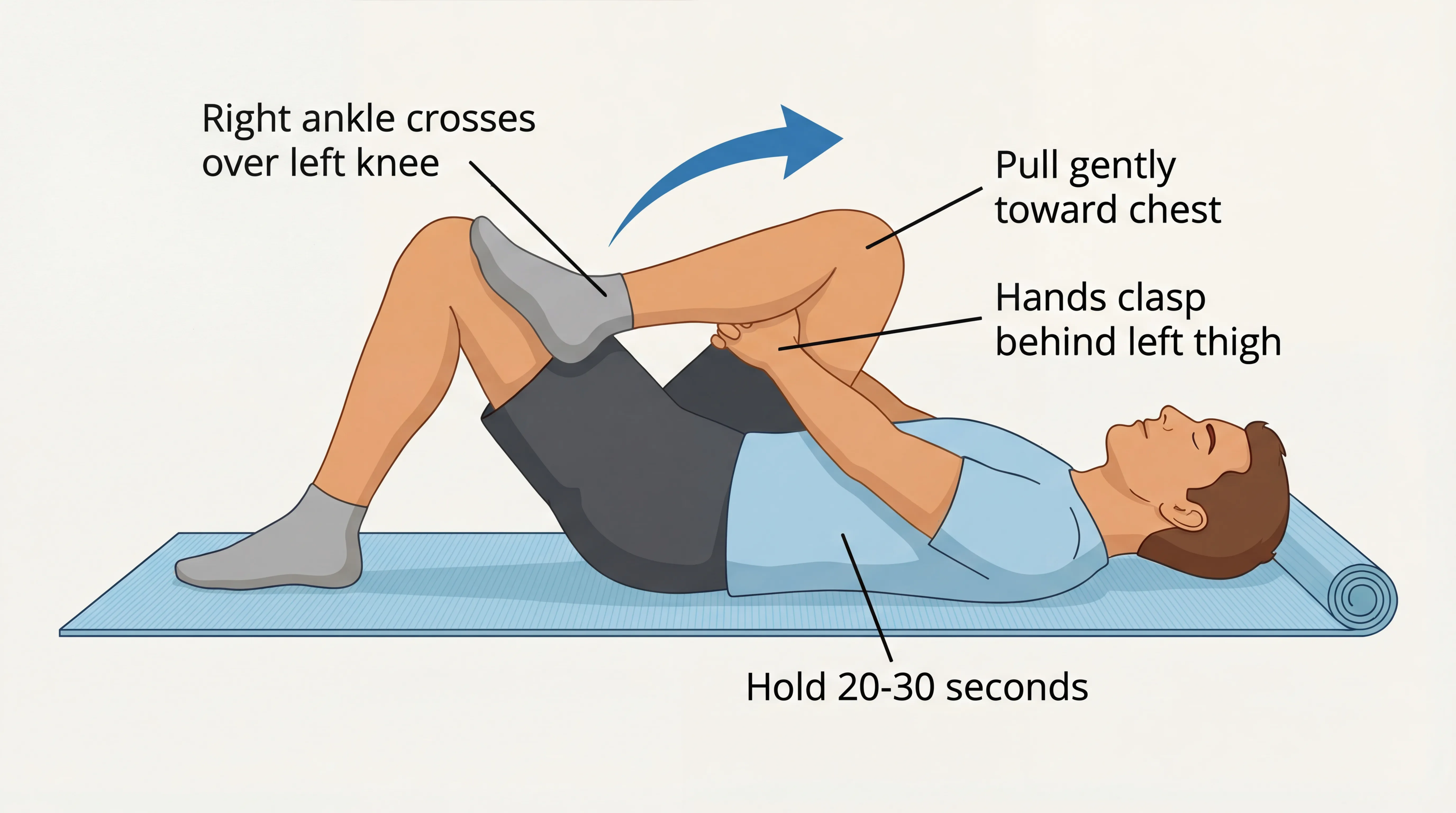
Lie on your back, bend the affected knee to 90 degrees, and cross it toward the opposite shoulder while rotating the foot outward. Reproduction of buttock or leg pain is the most specific piriformis self-test.
3. Seated piriformis stretch
Sit in a chair, cross the affected leg over the other knee, and lean your chest forward. If this reproduces your buttock or leg pain, it suggests piriformis involvement.
4. Straight leg raise
Lie flat on your back. Have someone slowly raise your straight leg (keep the knee locked). Pain that radiates down the leg between 30 and 70 degrees suggests nerve root compression from a disc problem. That range is where the nerve roots are under peak tension as they're drawn taut through the spinal openings; below 30 degrees the nerve has too much slack to be provoked.[2]
Still not sure?
That is common. Whether your pain started after a long drive on the Dolphin Expressway or a morning run in Crandon Park, our free Symptom Navigator quiz can help you narrow it down further.
Treatment Differences
Piriformis syndrome responds to targeted muscle release and hip mobility work. Disc problems need core stabilization and sometimes medical intervention. If you're treating the wrong one, you're wasting time and potentially making things worse, which is why getting the right diagnosis matters before anything else.
Sciatica
Because sciatica is a symptom, treatment depends entirely on identifying the underlying cause. See how TheraMax treats sciatica for condition-specific options.
Piriformis syndrome
First-line treatment focuses on piriformis stretches, hip-strengthening exercises, and reducing prolonged sitting. TheraMax robotic therapy is a strong fit because the condition is fundamentally muscular, designed to deliver precise pressure at depths difficult to reach manually. Caveat: if the tightness stems from a disc problem, treating only the muscle provides temporary relief. Learn more about TheraMax piriformis treatment.
Herniated disc
First-line care includes core stabilization and McKenzie extension exercises. Most herniated discs improve within six to twelve weeks, and roughly 10% require surgical intervention.[4] TheraMax plays a supportive role designed to help relieve the secondary muscular guarding that can amplify pain. See TheraMax for herniated discs.
Bulging disc
Conservative care centers on core strengthening, postural correction, and low-impact movement. Many bulging discs need no treatment at all, and continued movement often produces better outcomes than aggressive intervention. If back stiffness starts radiating into the leg or worsening with forward bending, that signals the bulge may be progressing and warrants professional evaluation. When symptoms persist, see TheraMax for herniated and bulging discs.
The biggest treatment mistake
In our Miami clinic near Coral Gables, the most common pattern we see is people who spent months treating piriformis tightness without addressing a disc contribution. The correct diagnosis is what makes treatment effective.
When to See a Professional
If you've been stretching and adjusting for a few weeks without real improvement, it's worth getting a professional evaluation. And certain warning signs mean you should skip the wait-and-see approach entirely.
Seek immediate evaluation if you experience progressive weakness in the leg or foot, numbness spreading to new areas, loss of bladder or bowel control (a medical emergency), or severe pain after significant trauma.
If you are still unsure what's behind your pain, a professional assessment can save months of trial and error. Call us at (786) 480-0026 or book online to get a clear answer.
Frequently Asked Questions
These are the most common questions we hear from people trying to distinguish between sciatica, piriformis syndrome, herniated discs, and bulging discs, and each answer addresses a point not covered in the comparison sections above.
1 Can you have both piriformis syndrome and a herniated disc at the same time?
2 Can a bulging disc turn into a herniated disc?
3 What affects how fast sciatica from a herniated disc heals?
4 Should I get an MRI before starting treatment?
5 Why do different doctors give different diagnoses for the same leg pain?
References
- The clinical features of the piriformis syndrome: a systematic review. Eur Spine J. 2010 ;19 (12) :2095-2109 . PubMed
- The test of Lasègue: systematic review of the accuracy in diagnosing herniated discs. Spine. 2000 ;25 (9) :1140-1147 . PubMed
- Herniated lumbar disc. BMJ Clin Evid. 2009 . PubMed
- An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014 ;14 (1) :180-191 . PubMed
- Bulging disk vs. herniated disk: What's the difference?. Mayo Clinic. 2024 . Source
